Men's Chest Contouring & Sculpting: Targeting Chest Fat & Enlarged Glandular Tissue
Discover effective chest contouring and sculpting solutions for men to reduce chest fat and enlarged glands to achieve a more defined, masculine chest.
Gynecomastia (pronounced guy-neh-co-mastia) is Greek for "women's breasts". The term was first coined by Galen, a second-century AD physician. It describes excess glandular and/or fatty breast tissues in man.
Also known as man boobs, gynecomastia is a benign enlargement of the male breast. Defined as the presence of abnormal proliferation of breast tissues in males, it is a common condition with varying prevalence across different age groups.
Studies suggest that a significant percentage of males experience it at some point, particularly during puberty and later in life. The prevalence can range from 32% to 65%, depending on the age and criteria used for definition[10].
Defined clinically by the presence of firm mass (glandular tissue) that extends concentrically from the nipples.
When both fat and firm mass (glandular tissue) are the cause.
Characterised by ONLY fat deposition WITHOUT the involvement of enlarged glandular tissue.
The self-check method:
Studies have shown the profound psychological impact that gynecomastia has on male sufferers. Body dissatisfaction has resulted in a high percentage of males with:
Gynecomastia (True and Mixed) is universally classified under “Gynecomastia Scale” under Grade I, II, III and IV, according to the severity of breast tissue enlargement.
.webp)
Small breast enlargement.
Localised button of tissue concentrated around the areola.
Less noticeable with clothing but evident when undressed.

Most common.
Moderate male breast enlargement.
Expands up to the width of the chest.
Loose skin may or may not be present.
.webp)
Moderate to significant enlargement.
Resembles a woman's breasts.
Often noticeable.
.webp)
Significant breast enlargement.
Substantial excess skin.
Severe and highly visible.
Giving the appearance of a feminine breast.
According to the National Institutes of Health Singapore, about 50% to 60% of adolescent males experience gynecomastia.
Causes
Male hormonal changes, resulting from the effect of an altered estrogen/androgen balance on the breast tissues.
Although it is not unusual for the condition to regress over time, this is unfortunately not always the case for some.
Teenagers may be uncomfortable discussing the issue and therefore may keep it from their parents and family members.
This can lead to long-term adverse effects such as low self-esteem, depression, and lack of body confidence.
Your child needs to understand that the issue can be resolved, and seeking a doctor's consultation is the best way to assess.

One of the most obvious signs is abnormal breast development.
An increase in size and changes in appearance, such as enlarged areolas.

The child may:

He may complain of:
Nearly 65% of men aged between 27 and 92 had some kind of gynecomastia.
Causes
In one of Dr Ivan Puah's studies in 2025, he analysed 602 patients treated for gynecomastia between January 2018 and December 2024 to prove that gynecomastia affects men of all ethnicities in Singapore — debunking stereotypes that single out one racial group.
The study identified the patient demographics of individuals who sought gynecomastia surgery from Dr Ivan Puah:
Understanding the anatomy of the gynecomastia gland guides a gynecomastia doctor to perform a more thorough and sufficient gland excision.
Ideally, the male chest should be flat with the pectoralis muscle accentuated. In the gynecomastia patient, the male breasts possess a more pyramidal shape with feminine features.

There are a couple of steps that Dr Ivan Puah will take to determine whether you have gynecomastia, which typically will include a physical examination of your chest area, along with questions about your medical history, so that he can plan a tailored treatment for you.
History and physical examinations are crucial elements when considering gynecomastia diagnosis[1].
Blood work may include liver function tests and assays for:
Gynecomastia surgery is recommended for:
Gynecomastia surgery can treat males with bilateral or unilateral gynecomastia, with protruding and prominent areolas. Before considering surgery, ensure that your weight is stable and you are in good general health without any serious underlying medical conditions.
Inform us about your medication usage, especially if you are taking any steroids or using anabolic steroids.
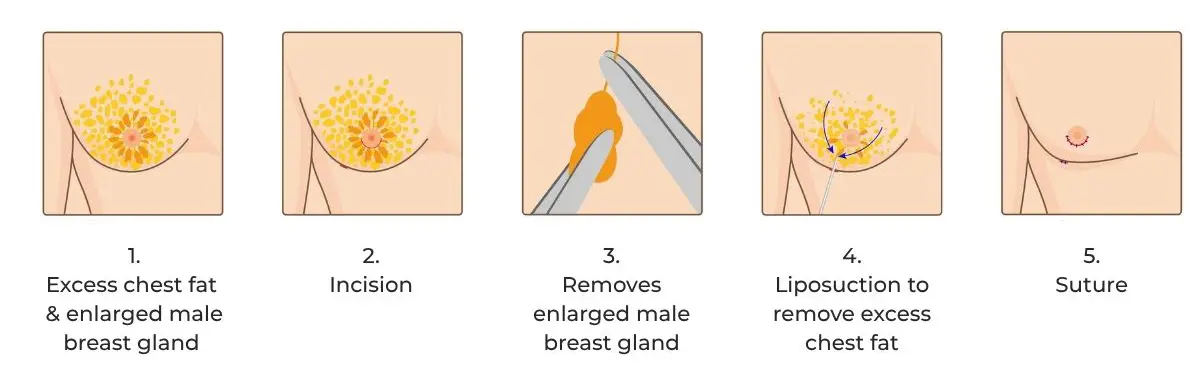
The surgery is carried out in an MOH-accredited Day Surgery. A team of experienced surgical personnel and anaesthesiologists will be working along side with Dr Ivan Puah during the surgery, to ensure optimal care and smooth surgery.
The patient will undergo twilight sedation (not GA) during the 2 to 2.5 hours procedure. Twilight sedation ensures the patient is comfortable and well-rested during the procedure while avoiding the possible anaesthesia complications associated with general anaesthesia.
Recovery time after surgery can vary from patient to patient, depending on the type of activities they plan to resume. In general, most patients can return to daily activities within 2 to 3 days, with little downtime.
Affected male breast tissues are removed.
Visible change before tissue swelling sets in.
Thick compression dressings are applied.
Wear the compression vest 24/7 for 2 months to control bruising and assist with tissue swelling.
Increase fluid intake.
Day 1
Follow post-op instructions as provided.
Discomfort from soreness and bruises are manageable.
Day 2 - 3
Resume work and normal daily activities.
Day 10
Stitch Removal and appointment for follow-up treatments are given. MLD Therapy is recommended.
Start the use of Amaris B. Scar Gel
Week 2
Swelling and bruising subside.
No upper body gym work until doctor's clearance.
Gentle swimming is allowed once your incisions have closed.
Week 3
Gradually resume low-impact exercise.
Week 6
Subject to recovery progress, most patients can resume gym work.
Week 8
Expect a flatter and more contoured chest shape.
Skin continues to tighten and improve.
Final review with Dr Ivan Puah to assess your before and after results.
Your final chest contour will gradually reveal itself over a period of 3 to 6 months as the swelling continues to go down with more defined chest contour.
Scars will begin to soften and fade during this time. It's important to know that this is a slow process, and it can take a year or more for them to reach their final, most subtle appearance.
When dealing with gynecomastia, selecting the right doctor is crucial.
Here are some key considerations when choosing a suitable gynecomastia doctor for your unique condition:
Should be experienced and performs at least 2 to 4 surgeries weekly.
Who has treated different gyno grades.
Gives you a clear explanation and does not brush off your issues and enquiries.
Ethical, empathetic, with good bedside manners, and is reassuring.
Confident with his results and can show you a wide range of cases he has done.
You are not overpromised on your results.
You have received a clear explanation on what is achievable and not.
The doctor's medical team are professional, helpful and reassuring.
Should be able to address and assist you with your inquiries confidently.
Insurance claim and Medisave coverage issues assistance, where needed.
Provide timely post-surgery advice.
As with any surgical procedure, there are inherent risks, which include but are not limited to adverse reactions to anaesthesia, infection, bleeding, or the formation of hematomas.
While the goal of any gyno doctor is to create a smooth and natural-looking chest contour, there is always a possibility of minor asymmetry, under-correction, or a subtle residual tissue presence. The formation of scars is an expected part of the healing process; however, every technical measure is taken by Dr Ivan Puah during surgery to minimise their appearance.
It is important to contextualise these risks: serious complications are exceedingly uncommon. This is supported by data[17], including a significant study of over 1,700 patients that demonstrated a very low rate of major postoperative issues.
Please be assured that your well-being is our utmost priority at Amaris B. Clinic. Our surgical protocols are meticulously designed to prioritise safety at every step.
Gynecomastia surgery has a high success rate based on years of patient data collected by Dr Ivan Puah and also according to international studies. International research[18] shows that an overwhelming majority of men (over 90%) are happy with their results from gynecomastia surgery.
While satisfaction is very high, it's also important to have a realistic outlook and discuss potential risks and long-term outcomes with Dr Ivan Puah for a complete picture.
To ensure optimal results and reduce post-surgery complications, it is crucial for the patient to diligently follow the pre-op and post-op instructions provided.
As stated in the American Society of Plastic Surgeons' Recommended Insurance Coverage Criteria for Third-Party Payers, which is used as a benchmark by most insurance companies to assess gynecomastia claims in Singapore and internationally, the recommended gynecomastia insurance claim for adolescents and adults varies.
Depending on the surgical indication, Singaporeans and Permanent Residents may be able to utilise a portion of Medisave, however, CHAS subsidies are not applicable.
What affects the cost?
Your total surgical fees vary based on several factors such as:
Unilateral or bilateral grade II or grade III gynecomastia present:
Unilateral or bilateral grade IV gynecomastia present:
Important consideration: Pain and discomfort due to the distention and tightness from the hypertrophied breast.
Unilateral or bilateral grade III or IV gynecomastia present:
Important consideration: Breast enlargement can lead to scarring that prevents tissue regression, causing pain and discomfort from swelling and tightness.
We provide before-and-after photos privately during your one-on-one consultation with Dr Ivan Puah. You will be able to view anonymised images of actual patients who had undergone gynecomastia surgery.
They allow you to:
Disclaimer: While these clinical visuals are shared in-clinic for your education, MOH strictly prohibits displaying before/after images in ANY public advertising (website, social media, brochures etc.). We fully comply to ensure ethical patient communication, no unrealistic outcome promises and protection of patient privacy. Visual examples are for educational reference only - individual results vary based on your unique condition.
Gynecomastia surgery is a significant investment for patients, encompassing financial, mental, and physical aspects. Now that you are free from gynecomastia, here are three essential tips to help you maintain the results.
Lifestyle
Team
Eat well
First thing to know: your body will form scar tissue as it heals. You can gently massage the area once Dr Ivan Puah gives you the green light. This helps to prevent raised or stiff scars from forming.
Other strategies you can adopt to take care of your surgical scars include:

Its gentle pressure helps to smooth out any scar formation.

Fresh scars can tan darker than your normal skin, so keep them covered or slather on that strong sunscreen.
Avoid outdoor activities that require you to remove your shirt for at least 6 months.
If unavoidable, apply sunscreen with SPF 50+ and use scar reduction gel/cream.

Silicone, in gel form or as self-adhesive sheets, has been used for decades to speed up scar fading and soften the look of the scars over time.

Manual Lymphatic Drainage (MLD) Therapy at Amaris B. can help to encourage blood flow, stimulate the healing process, improve skin texture, and minimise scar formation.

Scars need time to settle down and fade — we’re talking a full year or sometimes more before you see the final result.
If you’re really concerned about how things are looking or feeling down the line, have a chat with us at Amaris B.
There are in-office treatments such as laser scar removal therapy or steroid injections that can be helpful.
Post-op recovery is a journey, but taking these steps will help everything heal as smoothly as possible.
Dr Ivan Puah is an accredited liposuction doctor and Chairman of the Lipo Peer Review Committee in Singapore in Singapore with over two decades of clinical experience.
He has completed fundamental and advanced Vaser Liposuction body sculpting surgical training under Dr John Milard and Dr Alfredo Hoyos in Argentina and Colorado. He has also received dedicated gynecomastia surgery training in San Francisco.
Dr Puah marries the principles of science and art in his body contouring surgeries, delivering natural and optimal results for his patients.

No, being overweight is not the only cause of gynecomastia, although the more fat tissues you carry, the higher your chance of developing gynecomastia, so the problem tends to be prevalent among overweight men.
However, men in great shape also suffer from the condition because it is caused primarily by a hormone imbalance.
Is gynecomastia caused by genetics?
Gynecomastia is an endocrine system disorder that causes an enlargement in the size of male breast tissue and it can be caused by genetics.
Is gynecomastia an early sign of breast cancer?
Breast cancer is not only subjected to women as men can get them, although it accounts for only 0.2 percent of all malignancies in male patients.
Gynecomastia, however, is not a sign of developing breast cancer. Also, excessive breast development and breast cancer are not correlated.
Is gynecomastia caused by andropause (male menopause)?
According to statistics, male menopause or andropause happens when testosterone production drops in men aged 50 or older. Testosterone fuels changes during puberty and affects a man's mental and physical energy. It also regulates other vital evolutionary features.
As the levels of testosterone drop, it causes a hormonal imbalance, which may eventually lead to the development of gynecomastia.
I am overweight. How do I lose the fat and excess breast tissue?
For those who are overweight, it is assumed that they can lose the extra fat prevalent in the chest area with dieting and exercise, only to worsen the situation, causing the unflattering chest to appear more noticeable.
Maintaining a healthy weight and body is always recommended. If being overweight is an issue, do try to lose the extra weight. If you think you're suffering from gynecomastia, seek a qualified doctor's advice as soon as possible to safely and effectively address the issue.
Can I exercise or diet gynecomastia away?
Unfortunately, it is impossible to get rid of gynecomastia with exercise because the majority of the time, the problem is excess glandular tissue that no amount of exercise or healthy eating will eradicate.
In fact, many men have reported that as they lose weight, the gynecomastia looks worse because the fatty tissue around the gland shrinks and the gland subsequently stands out more, making the condition more prominent.
Can doing more chest exercise reduce the swollen man boobs?
Gynecomastia is caused by hormone imbalance, so while exercising is good, it does not resolve the underlying issue at all.
Can gynecomastia be treated?
Yes, the predominant treatment to deal with gynecomastia is surgical - gynecomastia surgery.
Are there any natural remedies for gynecomastia?
Despite what's being purported, there is no scientific evidence to prove that topical creams, fat freezing machines, fat reduction machines, or massage techniques can solve the condition permanently. Gynecomastia surgery is the option for surgical correction of gynecomastia.
Can food containing soy beans cause gynecomastia?
Soy contains isoflavones, a class of phytoestrogens which may mildly mimic the hormone estrogen. The effects of soy isoflavones on estrogen levels are complex, but in general, soy is safe to be consumed in moderation. Eggs, milk and other food products that contain hormones are safe for consumption when taken in moderation.
Can beer give you male boobs?
Hoppy beers like IPA (Indian Pale Ale) contain phytoestrogen, a plant-based estrogen hormone. The common myth is that drinking too much of them will cause estrogen levels to skyrocket. The phytoestrogen levels are too low to create any hormone imbalance. But still, consuming beers or any alcohol excessively can be detrimental to your overall health.
Can gynecomastia surgery be performed at the same time with another procedure?
Yes, full male body contouring is sought after by male patients, and they usually request for fat reduction of the face, abdomen and waists at the same time as their male breast reduction surgery.
What types of medications cause gynecomastia?
Following are some of the medications that can cause gynecomastia:
Does Amaris B. provide aftercare treatments?
At Amaris B. Clinic, aftercare significantly assists you with faster recovery and ensures optimum results. We have curated a bespoke aftercare program designed to help you with the healing process, such as manual lymphatic drainage massages, skin firming and many others.
Is recurrence of gynecomastia common after gynecomastia surgery?
Although rare, 10 percent of patients who have had surgery may experience a recurrence of gynecomastia. Ageing, hormonal changes, alcohol, opioids, and certain medications and drugs are usually associated with the onset of gynecomastia.
Can gynecomastia surgery only be performed by plastic surgeons?
No. As gynecomastia surgery involves liposuction and breast tissue removal, all doctors offering this service, including plastic surgeons alike, must meet the stringent criteria set by the board and be liposuction accredited by the Ministry Of Health Singapore. Dr Ivan Puah is one of the doctors to receive the accreditation.
Reference
[1] https://emedicine.medscape.com/article/1273437-overview
[2] Toorians AW, Bovee TF, De Rooy J, Stolker LA, Hoogenboom RL. Gynaecomastia linked to the intake of a herbal supplement fortified with diethylstilbestrol. Food Addit Contam Part A Chem Anal Control Expo Risk Assess. 2010 Jul;27(7):917-25. doi: 10.1080/19440041003660869. PMID: 20432093.
[3] Henley, D. V., Lipson, N., Korach, K. S., & Bloch, C. A. (2007). Prepubertal gynecomastia linked to lavender and tea tree oils. New England Journal of Medicine, 356(5), 479-485.
[4] Mathur R & Braunstein GD 1997 Gynecomastia: pathomechanisms and treatment strategies. Hormone Research 48 95-102.
[5] Svartberg J, Jorde R. Endogenous testosterone levels and smoking in men. The fifth Tromsø study. Int J Androl. 2007 Jun;30(3):137-43. doi: 10.1111/j.1365-2605.2006.00720.x. Epub 2006 Nov 27. PMID: 17163954.
[6] Rachdaoui N, Sarkar DK. Effects of alcohol on the endocrine system. Endocrinol Metab Clin North Am. 2013 Sep;42(3):593-615. doi: 10.1016/j.ecl.2013.05.008. PMID: 24011889; PMCID: PMC3767933.
[7] de Ronde W, de Jong FH. Aromatase inhibitors in men: effects and therapeutic options. Reprod Biol Endocrinol. 2011 June 21;9:93. doi: 10.1186/1477-7827-9-93. PMID: 21693046; PMCID: PMC3143915.
[8] Duca Y, Aversa A, Condorelli RA, Calogero AE, La Vignera S. Substance Abuse and Male Hypogonadism. J Clin Med. 2019 May 22;8(5):732. doi: 10.3390/jcm8050732. PMID: 31121993; PMCID: PMC6571549.
[9] Blau M, Hazani R, Hekmat D. Anatomy of the Gynecomastia Tissue and Its Clinical Significance. Plastic and Reconstructive surgery. Global Open. 2016 Aug;4(8):e854. DOI: 10.1097/gox.0000000000000844. PMID: 27622122; PMCID: PMC5010345.
[10] Braunstein GD. What Accounts for the Increased Incidence of Gynecomastia Diagnosis in Denmark from 1998-2017? J Clin Endocrinol Metab. 2020 Oct 1;105(10):e3810–1. doi: 10.1210/clinem/dgaa485. PMID: 32710775; PMCID: PMC7431205.
[11] Fu, D., Miao, H., Wang, Z., & Yang, C. (2025). Gynecomastia and Its Potential Progression to Male Breast Cancer: Mechanisms, Genetic Factors, and Hormonal Interactions. Critical Reviews in Oncology/Hematology, 104651.
[12] Mannix, J., Duke, H., Almajnooni, A., & Ongkeko, M. (2024). Imaging the Male Breast: Gynecomastia, Male Breast Cancer, and Beyond. RadioGraphics, 44(6), e230181.
[13] Grubstein, A., Dahan, M., Jomar, W., Friehmann, T., Tamir, S., Shochat, T., ... & Allweis, T. M. (2024). Screening Mammography for Males With Elevated Breast Cancer Risk, Mutation Carriers, and Gynecomastia. Clinical Breast Cancer, 24(6), e503-e508.
[14] Ambareen, S., Rani, K., Kerketta, Z. H., & Murari, K. (2024). Male Breast Cancer: A Retrospective Analysis of Clinical and Pathological Features at a Tertiary Care Center. Asian Pacific Journal of Cancer Care, 9(1), 3-7.
[15] Mannix, J., Duke, H., Almajnooni, A., & Ongkeko, M. (2024). Imaging the Male Breast: Gynecomastia, Male Breast Cancer, and Beyond. RadioGraphics, 44(6), e230181.
[16] Zheng, G., & Leone, J. P. (2022). Male breast cancer: An updated review of epidemiology, clinicopathology, and treatment. Journal of oncology, 2022(1), 1734049.
[17] Zavlin D, Jubbal KT, Friedman JD, Echo A. Complications and Outcomes After Gynecomastia Surgery: Analysis of 204 Pediatric and 1583 Adult Cases from a National Multi-center Database. Aesthetic Plast Surg. 2017 Aug;41(4):761-767. doi: 10.1007/s00266-017-0833-z. Epub 2017 Mar 24. PMID: 28341949.
[18] Taheri AR, Farahvash MR, Fathi HR, Ghanbarzadeh K, Faridniya B. The Satisfaction Rate among Patients and Surgeons after Periareolar Surgical Approach to Gynecomastia along with Liposuction. World J Plast Surg. 2016 Sep;5(3):287-292. PMID: 27853693; PMCID: PMC5109391.

Dr Ivan Puah's novel 360° Glandular Tissue Dissection (360°GTD®) technique minimises surgical invasiveness while achieving cosmetic results.


Dr Ivan Puah's novel 360° Glandular Tissue Dissection (360°GTD®) technique minimises surgical invasiveness while achieving cosmetic results.


Dr Ivan Puah's novel 360° Glandular Tissue Dissection (360°GTD®) technique minimises surgical invasiveness while achieving cosmetic results.
